Osteoarthritis When
Your Joints HurtOctober
2016
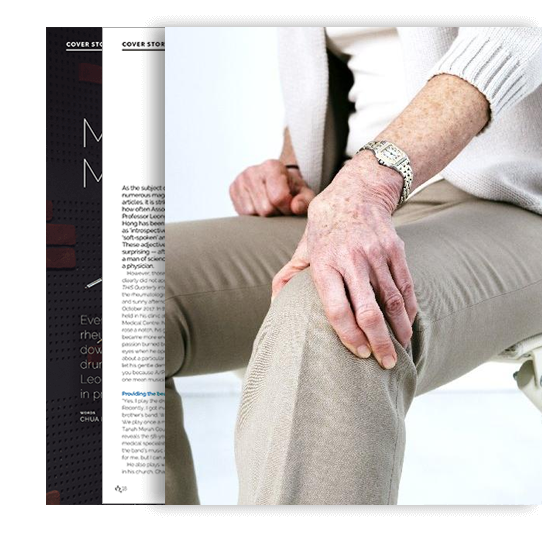
Even the strongest and healthiest bodies are subject to wear and tear, and this is why joints are susceptible to ostheoarthritis
A common ailment in the elderly, osteoarthritis or degenerative joint disease is the most prevalent form of arthritis. Affecting the joint cartilage, it causes stiffness and pain, worsening as the level of activity progresses through the day.
It also typically affects overweight people; the excess weight increases stress on weight-bearing joints such as the knees, hips and lower back. It doesn’t mean that osteoarthritis is exclusive to the elderly and overweight though; there are also variants such as primary or generalised osteoarthritis that are familial and start in the hand joints. In these patients, weight loading does not seem to be a major factor.
Osteoarthritis can be described as a disorder of cartilage metabolism, where patients are more prone to cartilage degradation. This is accelerated if they have previous joint injury, joint inflammation or increased weight loading if they are obese. In advanced cases, one can think of the condition as “joint failure” as in any other organ failure.